Level of need UK health
Climate change impacts on UK health
Climate change affects most health determinants by influencing the dayto-day weather conditions we experience. Climate change, both in the UK and abroad, can impact upon local health.
There are 3 main ways climate change can impact health:
- Effects of extreme weather, such as heatwaves, flooding, wildfire, storms, and drought on physical and mental health (for example injuries and trauma, heat-related illness), as shown in Appendix 1. Such events are expected to increase in frequency and severity in coming years
- Effects on the planet’s life-support systems, such as rising sea levels and safe water availability, changing patterns of zoonotic and vector-borne disease (for example malaria, dengue fever), reduced pollination, and crop failure leading to food shortages.
- Effects mediated by social systems, such as livelihood loss, rising prices of food and fuel, supply chain disruption, pressure on health and care services, conflict or forced migration.
Temperature changes
Older adults and those with chronic medical conditions are vulnerable to health harms from both hot and cold temperature extremes. Temperature related deaths will primarily affect those aged 85+ years.
Hotter temperatures can increase cardiovascular risk factors, such as poorer glycaemic control, increased blood pressure, increased cholesterol, and reduced exercise. Heat related risks will increase substantially as shown in Figure 4, however the North East is predicted to have the lowest levels of heat-related deaths in the UK
Cold-related deaths will be a greater concern for the region as the risks are already present in England and will continue.
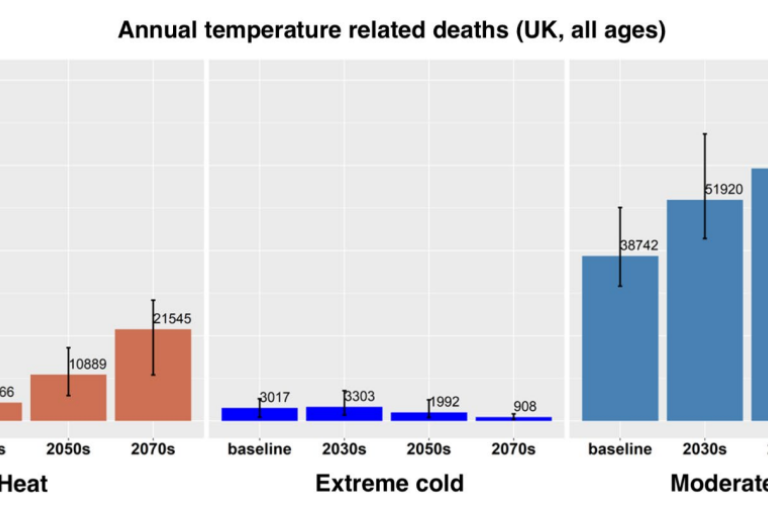
Figure 3: Project UK heat and cold deaths for all ages (Baseline= 2007-2018), UKHSA
Flooding
Flooding can pose multiple risks to health, such as deaths from drowning and physical injury through contact with flood waters or car accidents. Injuries can also occur from cleaning after a flood (including CO poisoning). Flooding increases the risk of hypothermia and infectious disease outbreaks, as well as exposure to industrial/agricultural chemicals. The risk of mental health impacts, such as PTSD, depression, and anxiety, is also increased following a flood.
There is predicted to be an increase nationwide of those at risk to flooding by 2080 as shown in Figure 4. Coastal communities are particularly at risk. Flooding does not impact populations equally, having very localised effects.
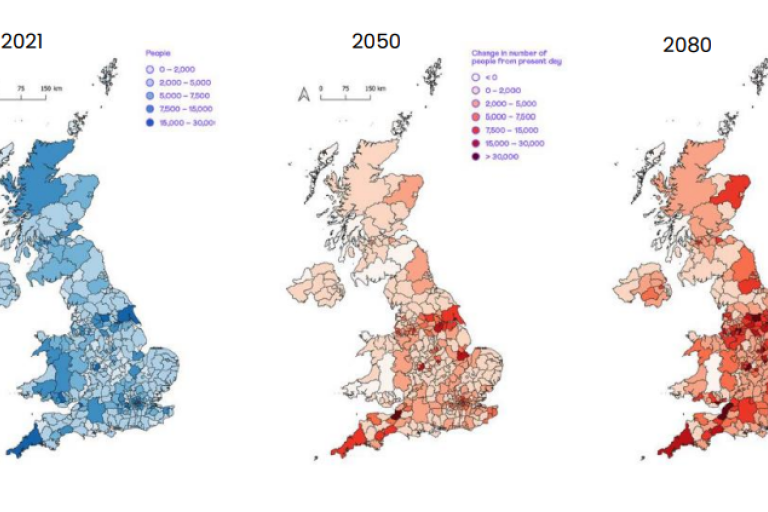
Figure 4: Change in the number of people at risk from flooding, UKHSA
Air pollution
Poor air quality can increase the risk of respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), and cardiovascular diseases, such as hypertension, heart attacks, and stroke. 0–19 year-olds can be susceptible to asthma due to particulate air pollution and some premature deaths in over 65’s can be associated with particulate air pollution .The Chief Medical Officer’s Annual Report on Air Pollution further summarises the health impacts of air pollution.
The most common sources of air pollution are shown in Figure 6. Air pollution is affected by both local conditions as well as transboundary conditions. Contributions from transport in the Benelux region, large dust events from the Sahara, wildfires, and volcanic eruptions can all contribute to air pollution in the UK.
Communities who work or live close to major roads, such as the A1, A19, or Coast Road, will be more exposed to higher concentrations of air pollution. Low-income communities are often susceptible to the effects of air pollution
The primary pollutants monitored in North Tyneside are NO2, PM2.5, and PM10. These are primarily traffic related emissions. A 2023 report on air pollution within North Tyneside showed across all monitoring locations in the Borough, average NO2 levels were recorded to be below the UK air quality objectives.
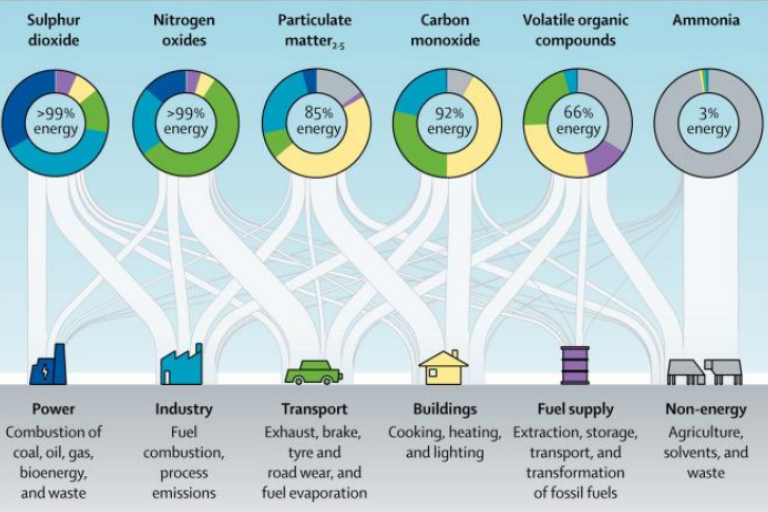
Figure 5: Sources of air pollution, Lancet, 2017
Outdoor airborne allergenic pollen and fungal spores
Aeroallergens are airborne particles that can cause or exacerbate allergic disorders, including pollen and fungal spores. Aeroallergens can trigger hay fever and exacerbate asthma which affects about 11% of the UK population.
Data remains limited, but there is suggestion of increased production of certain aeroallergens or longer seasons of exposure. Evidence suggests that there is likely to be a longer fungal spore season due to hotter summers with more intense periods of rainfall.
Infectious and vector borne diseases
Many infectious diseases are climate sensitive. Warmer temperatures can alter the geographical distribution of infectious diseases and extend the transmission periods of some diseases. Impacts of climate change on infectious diseases is unclear, but there is strong evidence that risk from Salmonella, Campylobacter, and Vibrio spp may increase in the future. There is likely to be minimal change to influenza from climate change.
Tick and mosquito borne illnesses are likely to become more common in England, which may affect areas in the South of the UK first. Tick numbers are already increasing in the UK with some increase in Lyme disease and tick-borne encephalitis seen. There is concern that an invasive mosquito species may establish in the UK, with risk of dengue fever, chikunmgunya, Zika, and West Nile virus.
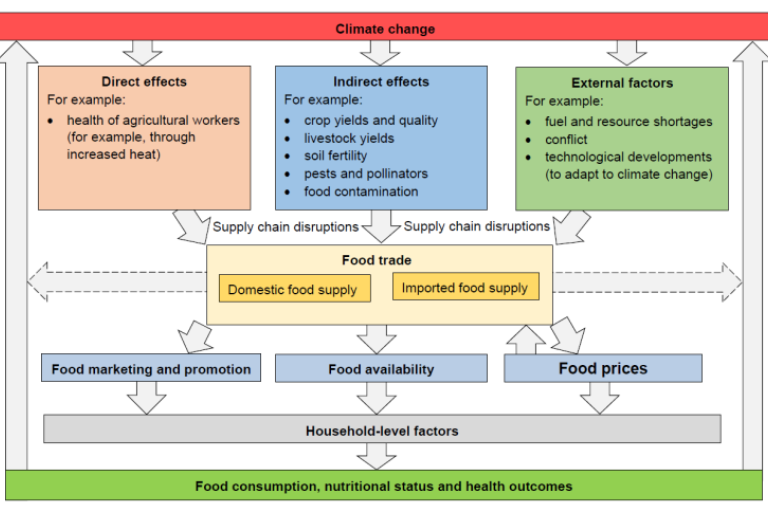
Food systems
The impact of climate change on food supply is shown in Figure 7.Risk to food supplies will likely increase global food insecurity in the future. The key food groups that would particularly fall short in supply in England, as compared to recommended dietary guidelines, include fruit and vegetables, starchy root vegetables, legumes, and fish.It is predicted that domestic supply may reduce over time, making England reliant on imports, some of which are from climate vulnerable countries.
The Lancet has vocalised concerns that low- and middle-income countries may see malnutrition due to crop failures and yield decline whilst high income countries may see obesity due to rising due to costs of fresh fruits and vegetables.
Wildfires
Wildfires can present a range of hazards that can cause injury or death, including suffocation, burns, electrocution, and injuries caused by unstable infrastructure. People may be exposed to hazardous substances from building materials, as well as biological materials from soiled and water damaged constituents.
Droughts
Although still rare, drought occurrence is increasing in the UK. Droughts can impact health directly as they may affect water quality and quantity, and compromise crop yields, with implications for food supply and nutrition. Droughts also have indirect effects, for example on vector-borne diseases by influencing vector habitat, and have been linked to biodiversity loss, wildfires, increased concentrations of certain allergens, and harmful mental health impacts.
Chemical exposure
Changes in temperature, precipitation, humidity, wind conditions, erosion, and extreme events due to climate change may affect the fate and behaviour of chemicals in the environment (atmosphere, water, soil, sediment). Climate change is likely to increase the release of chemicals, including contaminant discharge from polar ice and high-altitude glaciers, volatilised persistent organic pollutants (POPs) and pesticides into the atmosphere, increased agricultural related chemical exposure as well as soil and groundwater conditions due to changing crop yields, and increased exposure of industrial site chemicals from extreme weather.
Solar radiation
Sunlight exposure is needed for human health. It is needed for healthy bones, Vitamin D status, cardiovascular and metabolic health, melatonin regulation for quality sleep and serotonin regulation for improved mental health. Underexposure can result in Vitamin D deficiency, whilst overexposure can lead to skin cancers, sunburn, cataracts, premature skin ageing and altered immune response. Increasing UV radiation exposure could potentially have mixed health benefits.
